Dr. Williams' Urology Resource
A Guide to Men's Health, Reproductive Medicine, and Microsurgery
Vasectomy Reversal
Approximately 5% of men will decide to have more children after a vasectomy. Reasons for this can include divorce/remarriage, desire to have more children, or loss of a child.
Regardless of the reason, a man can change his mind, and in the absence of any female fertility problems, microsurgical vasectomy reversal is the most cost-effective way to get pregnant after a vasectomy, especially when it is done correctly the first time.
Choosing a microsurgeon who specializes in vasectomy reversal is important!
Microsurgical vasectomy reversals are generally performed as a same-day surgery at an outpatient surgery center. Proper recovery time after vasectomy reversal is as important as the surgery itself. Antibiotics and pain medication are prescribed after vasectomy reversal. Ice packs for the first couple of days will reduce pain and swelling from the vasectomy reversal. It is important to wear a scrotal supporter during the first 2 weeks after a vasectomy reversal and to abstain from sexual activity and other strenuous activities for during this time. This is recommended to allow the delicate microsurgical reconstruction to heal. It is also important to resume regular sexual activity after those first two weeks following vasectomy reversal.
The first semen analysis is typically checked 4-6 weeks after the vasectomy reversal. Anti-inflammatories may be prescribed if there is still evidence of swelling on examination or inflammatory cells in the semen.
Pregnancy outcomes are dictated by the type of vasectomy reversal that is employed (microsurgical vs. non-microsurgical vasectomy reversal and vasovasostomy vs. epididymovasostomy) as well as the age of the female partner. Studies have shown pregnancy rates of 50-60% after vasectomy reversal when female age is less than 40. These rates drop to under 15% when female age is greater than 40.
Click here to watch Dr. Williams perform a microsurgical vasectomy reversal (vasovasostomy)
Microsurgical Vasovasostomy
(Standard Vasectomy Reversal)Vasovasostomy is one technique of vasectomy reversal that refers to sewing the two cut ends of the vas deferens back together. It is performed only when sperm are found inside the testicular end of the vas deferens. Use of the operating microscope to reconstruct the vas deferens in 2 layers under high-power magnification results in superior outcomes over standard techniques of vasectomy reversal. If it is possible to perform a microsurgical vasovasostomy on both the left and right sides, there should be a >95% chance of having sperm return to the semen after this type of vasectomy reversal.
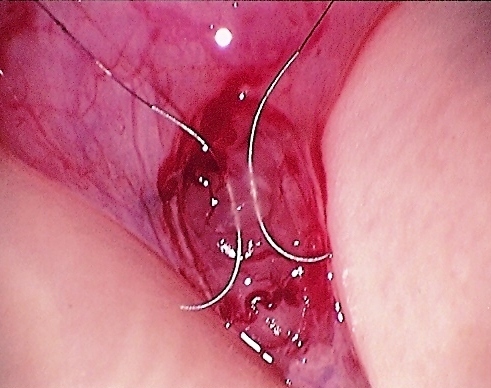
The two ends of the vas deferens are brought into proximity with each other at the beginning of a vasectomy reversal. Here, the back side of the inner and outer layers have been sewn together with 9-0 and 10-0 nylon sutures. The purple dots mark the edges of the outer layer.
The remaining 10-0 nylon sutures are placed within the inner lumen of the two ends of the vas deferens for the vasectomy reversal.
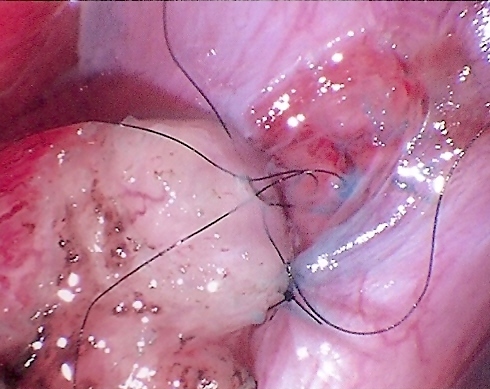
The inner layer sutures are tied for the vasectomy reversal.
The edges of outer layer are then brought together with interrupted 9-0 nylon sutures to complete the 2-layer, water-tight anastamosis. This completes the vasectomy reversal.
Microsurgical Epididymovasostomy
(Advanced Vasectomy Reversal)Although both the time interval since the vasectomy as well as certain findings on physical examination can help to predict the presence or absence of sperm at the time of vasectomy reversal, you don't really know for sure until the time of surgery when the fluid is examined under the microscope.
For this reason, it is critical that your surgeon has been trained in microsurgery and knows how to perform the complex epididymovasostomy type of vasectomy reversal when necessary.
At the time of vasectomy reversal, if no sperm are found in the testicular end of the vas deferens, then an obstruction has occurred further upstream of the vasectomy site, typically at the level of the epididymis. This phenomenon is referred to as an "epididymal blowout".
Performing a vasovasostomy in this setting would result in a failed vasectomy reversal.
In such cases, the more complex epididymovasostomy, or "bypass procedure" must be performed to reverse the vasectomy. This procedure involves connecting the vas deferens directly to the delicate tubules of the epididymis.
If it is necessary to perform an epididymovasostomy on both sides, success rates drop to 50-60%. This occurs primarily because the tubes of the epididymis are only one-fifth the size of the vas deferens. Most surgeons will recommend sperm cryopreservation for backup at the time of vasectomy reversal if bilateral epididymovasostomy is necessary.
Epididymovasostomy can only be performed using an operating microscope, and few urologists have been fellowship-trained to perform this complex vasectomy reversal procedure. Make sure that yours does!
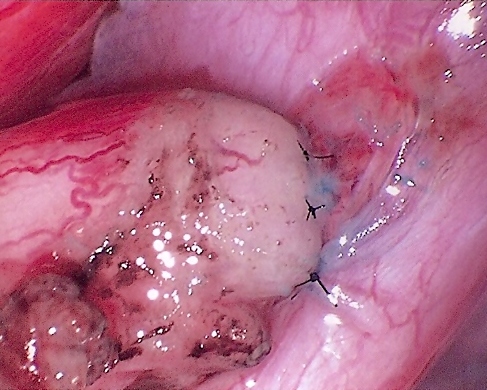
Two double-armed 10-0 nylon sutures are pre-placed to perform an intussusception epididymovasostomy. The tubule is then opened and the fluid is examined under light microscopy. If motile sperm are seen, the vasectomy reversal is continued at this site. If no sperm or non-motile sperm are seen, then another tubule is selected and examined until high-quality sperm are found.
Next, the abdominal end of the vas deferens is brought into proximity with the epididymal tubule. The previously-placed 10-0 nylon sutures are then placed into the lumen of the vas deferens to start the vasectomy reversal.
The 10-0 nylon sutures are tied, thereby completing the intussusception portion of the epididymovasostomy (advanced vasectomy reversal).
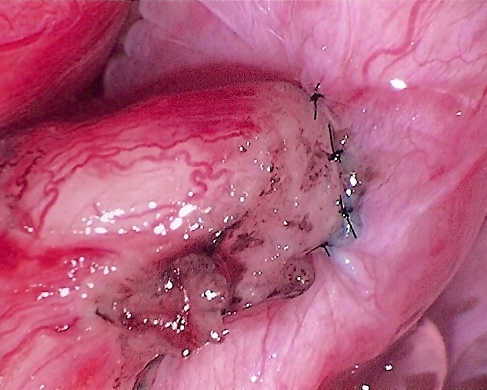
The outer layer of the vas deferens is sewn to the tunica of the epididymis to complete the vas-to-epididymis microsurgical vasectomy reversal.
Microsurgical Epididymal Sperm Aspiration (MESA)
An alternative to vasectomy reversal is to obtain sperm from the epididymis and use it for in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI). Once sperm are obtained, they may be frozen (cryopreserved) and used at any time in the future for IVF/ICSI.
Click here to watch Dr. Williams perform a microsurgical epididymal sperm aspiration
Copyright 2009 Williams Urology. All rights reserved.